The Lung Volume Reduction Program at Weill Cornell Medicine comprises of a multidisciplinary team of experts who share their clinical expertise in providing the patient the best possible recommendation and treatment plan for severe emphysema. Whether it is valves for bronchoscopic lung volume reduction, a minimally invasive lung volume reduction surgery, or referral for lung transplantation, patients who come to our program are guaranteed to receive highest level of care and personalized treatment approach.

“If patients are selected for valve procedure, they first undergo bronchoscopy under general anesthesia to examine the airway passages and ensure anatomy is favorable for the procedure.” says Dr. Eugene Shostak, an Interventional Pulmonologist and an Assistant Professor of Medicine in Cardiothoracic Surgery. “During bronchoscopy we also assess for presence of collateral ventilation, or communication of air between the target lobe and the adjacent areas of the lungs. If collateral ventilation is present, valves are not inserted as there would be little likelihood in successfully closing the lobe. Collateral ventilation is assessed using Chartis device, or a catheter that is capable of measuring flow of air with a balloon on its tip. Below diagram demonstrates two examples of what can be seen during collateral ventilation assessment.
“After placement of endobronchial valves we observe patients in the hospital for several days. Although individual results vary, many patients experience improvement in respiratory symptoms within few weeks."
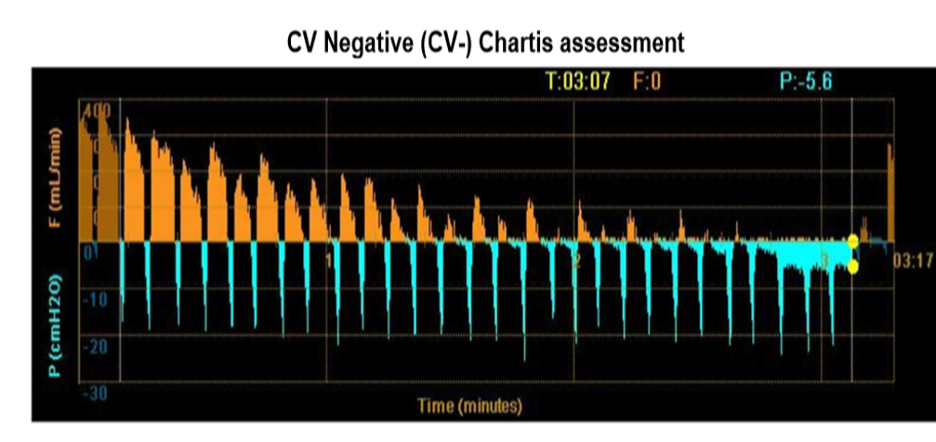
Diagram demonstrates reduction of air flow (yellow graph) suggestive of intact fissure. Absence of collateral ventilation (CV negative assessment) is a predictor of successful endobronchial valve procedure.
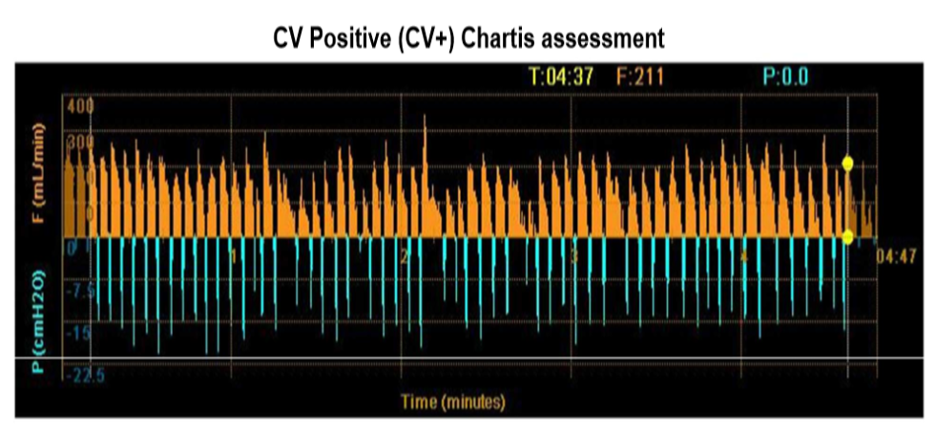
Diagram demonstrates no reduction of air flow (yellow graph) suggestive of incomplete fissure. Presence of collateral ventilation (CV positive assessment) would not result in successful lung volume reduction procedure and valves are therefore not inserted.

“When patients are felt to benefit from lung volume reduction procedure but do not qualify for endobronchial valves, they may be offered surgical lung volume reduction” says Dr. Jeffrey Port, Professor of Cardiothoracic Surgery with expertise in performing lung volume reduction surgery. “ These procedures are performed using minimally invasive techniques through 3 small incisions typically on the side that is most affected by emphysema. Every patient is discussed in front of a multidisciplinary team which allows us to recommend the best option for an intervention”
“Every patient who meets the clinical criteria for bronchoscopic lung volume reduction must have a CT scan of the chest to further assess eligibility”, says Dr. Daniel Green, Associate Professor at the Department of Radiology and an expert in thoracic imaging at Weill Cornell Medicine. “The important CT criteria for qualification are the severity and distribution of emphysema and the completeness of the fissures. Fissures are thin clefts that separate each lung into individual lobes. The right lung typically has two fissures and three lobes (upper, middle, and lower), and the left lung typically has one fissure and two lobes (upper and lower). Complete, or fully intact, fissures increase the likelihood of a successful outcome following endobronchial valve placement. Incomplete fissures, however, are common and allow collateral ventilation from one lobe to an adjacent lobe. While incomplete fissures have absolutely no significance for most people, they can prevent a lobe from collapsing after valve placement and therefore result in patients being considered ineligible for endobronchial valves.
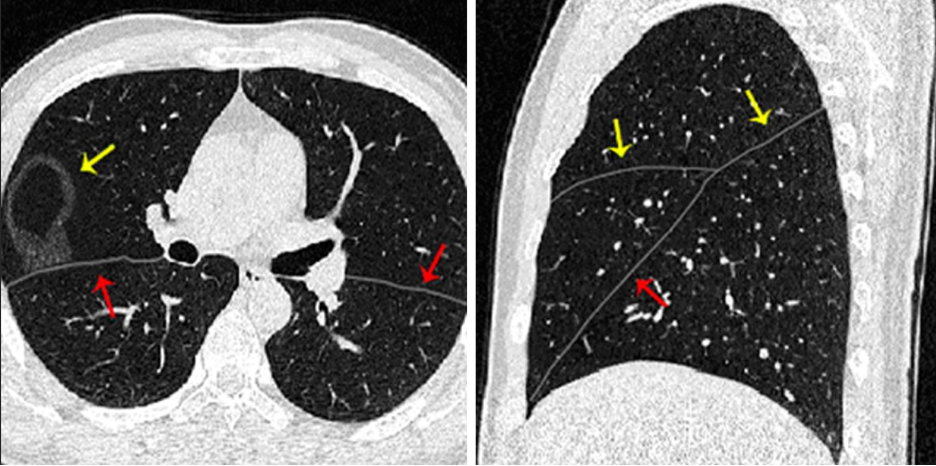
Arrows depict fissures, which separate various lobes of the lung and are important predictors of the success of bronchoscopic lung volume reduction procedure

“Here at Well Cornell Medical Center we are fortunate to use 3D V/Q SPECT-CT, which is the newest imaging method that offers anatomical and functional data on the amount of blood getting to the lungs” says Dr. Silvina Dutruel, Assistant Professor at the Department of Radiology specialized in Nuclear Medicine and Body Imaging. “As pioneers of this technology in New York City, our nuclear medicine specialists use a novel artificial intelligence-based software to estimate the percentage of blood that is distributed to each lobe of the lung. Compared to the conventional 2D perfusion scan, 3D V/Q SPECT-CT imaging offers a more accurate identification of how blood flow is distributed among individual lobes of the lung. This degree of precision improves our ability to more accurately select the best target for endobronchial valve procedure.”
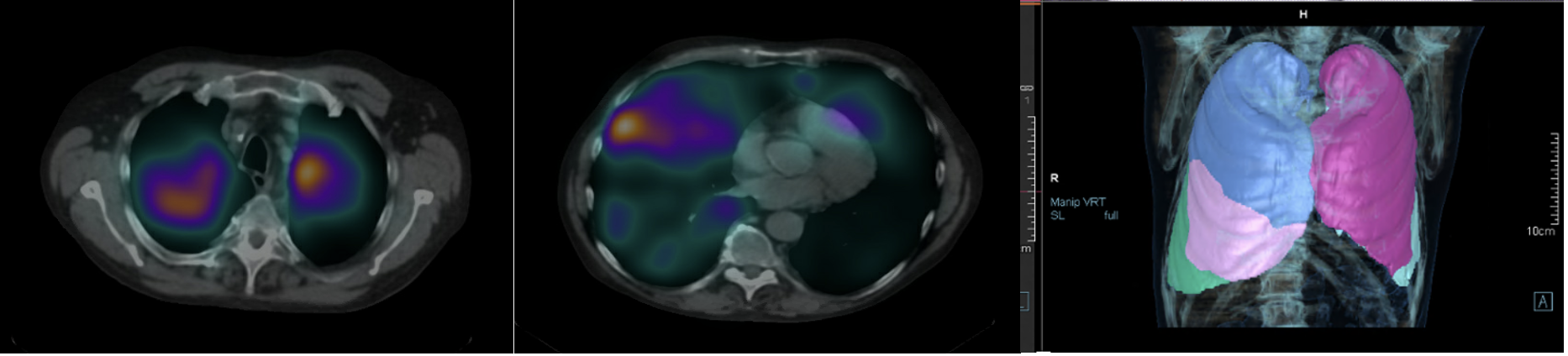
SPECT/CT images with different colors to identify blood flow to the lobes of each lung.